We use cookies to enhance your browsing experience and analyze the performance of our website. By clicking Continue, you agree to the use of cookies. For more information, please see our Privacy Policy or update your Cookie Preferences.

The Coeliac Profile is a blood test that uses widely accepted immunologic biomarkers to aid in the diagnosis of Coeliac disease (CD). The markers include Total IgA, Anti-Tissue Transglutaminase IgA (tTG IgA) and IgG (tTG IgG), Anti-Deamidated Gliadin IgA (DGP IgA) and IgG (DGP IgG), and reflex Anti-Endomysial IgA (EMA IgA).
Coeliac disease is defined as an autoimmune enteropathy of the small intestine, caused by exposure to dietary gluten in genetically pre-disposed individuals. In susceptible individuals, gluten ingestion generates an inflammatory reaction predominantly centered in the upper parts of the small intestine. This mucosal injury will eventually reduce the intestinal absorptive area and interfere with uptake of micronutrients.2
Testing should be performed while the patient is still on a gluten-containing diet.1 The exception is follow-up testing for monitoring treatment efficacy.
The Coeliac Profile can be ordered as a stand-alone profile or ordered together with other profiles. Often times, clinicians will order several smaller profiles together in order to see a more complete picture of the patient's immune mediated response. Profiles that can be ordered together include:
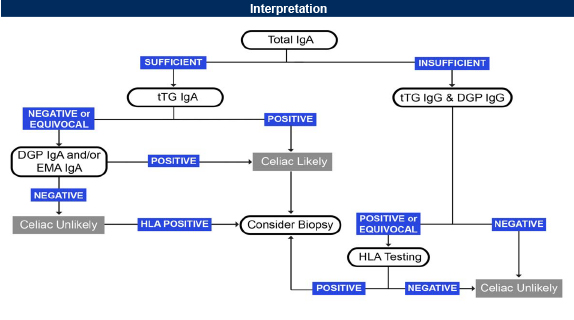
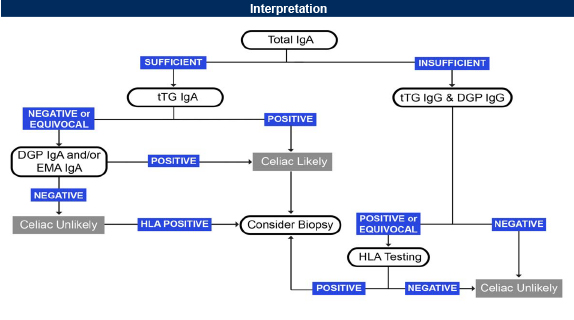
Intestinal biopsy is considered the gold standard for the diagnosis of Coeliac disease. International guidelines suggest that measuring immunologic analytes and genetic markers are favored to increase detection of CD. The European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) introduced a revised guideline for CD in children based on the optimisation of antibody assays. According to this guideline, children can be diagnosed with CD without a duodenal biopsy when presenting with suspicious symptoms, a strongly elevated tTG-IgA (>10 confirmed cut-off value), confirmed by a positive EMA-IgA on a separate occasion, and positive genetic testing (HLA-DQ2 and /or HLA-DQ8).5 Genova does not offer the HLA-DQ2/DQ8 genetic markers. Genova offers an interpretive algorithm to aid in assessing likelihood of disease:
Coeliac disease is an autoimmune condition where the body's immune system attacks the small intestine after being exposed to the food component gluten. This results in malabsorption of nutrients and symptoms such as diarrhoea, abdominal pain, weight loss, and bloating. This simple blood test can help your provider determine if further testing is necessary and develop a tailored food plan specific to your needs and symptoms.
We have many resources to help make your testing experience a success. Review the Test Preparation tab to learn more about the collection process.
Certain medications may impact test results. Please note that the reference ranges were established based on patients taking no medications or supplements. In some instances, it is unknown what potential impact a medication may have on test results. Genova never recommends that patients discontinue medically necessary medications or supplements in order to complete testing. There may be times when a patient may stay on a medication or dietary supplement during testing in order to evaluate its effectiveness. The recommendation to discontinue any substance is intended to establish a baseline finding. If you choose to discontinue a medication, a good rule of thumb is to take the biological half-life of the drug times 5 to allow for 'clearance' before testing. With certain medications, the drug itself may have cleared the body, but the effect of the medication may be longer lasting.
The following medications may influence the antibody test results; they would not be expected to interfere with the ability to run the assay itself:
These medications can either increase or decrease immunoglobulin levels and may result in false positive or false negative test results. Omalizumab is a monoclonal antibody designed to bind to free serum IgE, which may influence test results. Heparin interferes with the measurement of tissue transglutaminase (tTG) antibodies on the coeliac panel.
The following medications DO NOT interfere with testing or influence biomarker levels: antibiotics, antihistamines, antidepressants. Antihistamines and antidepressants are known to interfere with skin prick testing, not blood testing for allergies.
Clinicians may use the allergen-specific IgE antibody test to monitor response to immunotherapy (desensitization).
Important: If a patient has a known IgE-mediated food allergy, Genova DOES NOT recommend exposure to the food that may cause a reaction.
When testing for food antibodies, it is suggested that the patient eat a variety of foods for 2-3 weeks prior to testing (except for foods that are known to cause severe reactions). Doing so will help to ensure the presence of antibodies to problematic foods.
It is also important to remember that IgE antibodies have a circulating half-life of 1-5 days, so any reaction shows current exposure to the antigen, meaning exposure within the several days immediately prior to collecting the test sample. The circulating half-life of IgG is approximately 21-24 days, which means that by approximately 3 months, antibodies to a particular food may be absent if the food has not been consumed by the patient. In other words, if the patient has not consumed the food prior to testing, no reaction to that food would be expected.
When running the Coeliac Profile, it is important to note that antibodies will only be present if the patient has consumed gluten prior to testing. If the patient is already on a gluten-free diet, genetic testing of the HLA DQ2/DQ8 genes may be helpful. According to the American College of Gastroenterology, a proposed gluten challenge after being gluten-free involves eating 3 grams of gluten daily for 8 weeks prior to testing. However, diagnostic changes are seen in most coeliac disease patients after as little as 2 weeks of gluten ingestion.1
It is recommended that a child be at least 1 year old before testing for IgG antibodies in order to eliminate the possibility of maternal antibodies influencing the results. Studies are lacking on the transfer of food-specific antibodies and/or the clinical significance of these maternal antibodies measured in the child's serum.
IgE antibodies do not cross the placenta, so there is no age restriction for IgE testing. According to Medscape, "For immunoglobulin (Ig) E-mediated allergy, there is no minimum age for testing, although it is important to consider age-related changes in patterns of sensitization. Sensitization to foods can occur in babies who are only a few weeks old. On contrast, it is unusual to develop sensitization to respiratory allergens before 2 or 3 years of age. Furthermore, in preschoolers, sensitization to indoor allergens (e.g., cat, dog, dust mites) is more common than sensitization to pollens. Considering these patterns, it is certainly reasonable to test children for food-specific IgE in early infancy if the history suggests food allergy."2
Breastfeeding can result in the transfer of maternal IgG and IgA antibodies to the child. However, studies are lacking on the transfer of food-specific antibodies and/or the clinical significance of these maternal antibodies measured in the child's serum.
The immune system continues to develop into childhood. Therefore, the clinical applicability of test results in pediatric patients may be unclear. What may be interpreted as an abnormal result for an adult, may be normal for an infant's developing immune system. This can be the case with other immune testing, including stool calprotectin and stool eosinophil protein X (EPX), where elevations would be expected in a healthy infant, but abnormal in an adult.
Antibody testing may be inaccurate if the patient has liver disease, severe renal disease, protein-losing enteropathy, HIV infection, or other immunodeficiencies. In patients with selective IgA deficiency, coeliac disease testing should include the IgG antibody against tissue transglutaminase (tTG) and deamidated gliadin (DGP) since the IgA antibody may not be detected or may be very low.
Viruses such as Epstein-Barr virus (EBV), rubella, and cytomegalovirus (CMV) can be associated with lower antibody levels.
Results may be skewed in patients with rheumatological pathologies associated with the production of heterophilic antibodies, such as rheumatoid factor (RF).
Diseases associated with a false positive tissue transglutaminase (tTG) IgA antibody on the coeliac test may include type 1 diabetes, autoimmune liver disease, primary biliary cirrhosis, inflammatory bowel disease, connective tissue diseases, and HIV infection. Genetic testing of the HLA DQ2/DQ8 genes may be helpful in these patients.
The Coeliac Profile is a blood test that uses widely accepted immunologic biomarkers to aid in the diagnosis of Coeliac disease (CD). The markers include Total IgA, Anti-Tissue Transglutaminase IgA (tTG IgA) and IgG (tTG IgG), Anti-Deamidated Gliadin IgA (DGP IgA) and IgG (DGP IgG), and reflex Anti-Endomysial IgA (EMA IgA).
Coeliac disease is defined as an autoimmune enteropathy of the small intestine, caused by exposure to dietary gluten in genetically pre-disposed individuals. In susceptible individuals, gluten ingestion generates an inflammatory reaction predominantly centered in the upper parts of the small intestine. This mucosal injury will eventually reduce the intestinal absorptive area and interfere with uptake of micronutrients.2
Testing should be performed while the patient is still on a gluten-containing diet.1 The exception is follow-up testing for monitoring treatment efficacy.
The Coeliac Profile can be ordered as a stand-alone profile or ordered together with other profiles. Often times, clinicians will order several smaller profiles together in order to see a more complete picture of the patient's immune mediated response. Profiles that can be ordered together include:
Intestinal biopsy is considered the gold standard for the diagnosis of Coeliac disease. International guidelines suggest that measuring immunologic analytes and genetic markers are favored to increase detection of CD. The European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) introduced a revised guideline for CD in children based on the optimisation of antibody assays. According to this guideline, children can be diagnosed with CD without a duodenal biopsy when presenting with suspicious symptoms, a strongly elevated tTG-IgA (>10 confirmed cut-off value), confirmed by a positive EMA-IgA on a separate occasion, and positive genetic testing (HLA-DQ2 and /or HLA-DQ8).5 Genova does not offer the HLA-DQ2/DQ8 genetic markers. Genova offers an interpretive algorithm to aid in assessing likelihood of disease:
Coeliac disease is an autoimmune condition where the body's immune system attacks the small intestine after being exposed to the food component gluten. This results in malabsorption of nutrients and symptoms such as diarrhoea, abdominal pain, weight loss, and bloating. This simple blood test can help your provider determine if further testing is necessary and develop a tailored food plan specific to your needs and symptoms.
We have many resources to help make your testing experience a success. Review the Test Preparation tab to learn more about the collection process.
Certain medications may impact test results. Please note that the reference ranges were established based on patients taking no medications or supplements. In some instances, it is unknown what potential impact a medication may have on test results. Genova never recommends that patients discontinue medically necessary medications or supplements in order to complete testing. There may be times when a patient may stay on a medication or dietary supplement during testing in order to evaluate its effectiveness. The recommendation to discontinue any substance is intended to establish a baseline finding. If you choose to discontinue a medication, a good rule of thumb is to take the biological half-life of the drug times 5 to allow for 'clearance' before testing. With certain medications, the drug itself may have cleared the body, but the effect of the medication may be longer lasting.
The following medications may influence the antibody test results; they would not be expected to interfere with the ability to run the assay itself:
These medications can either increase or decrease immunoglobulin levels and may result in false positive or false negative test results. Omalizumab is a monoclonal antibody designed to bind to free serum IgE, which may influence test results. Heparin interferes with the measurement of tissue transglutaminase (tTG) antibodies on the coeliac panel.
The following medications DO NOT interfere with testing or influence biomarker levels: antibiotics, antihistamines, antidepressants. Antihistamines and antidepressants are known to interfere with skin prick testing, not blood testing for allergies.
Clinicians may use the allergen-specific IgE antibody test to monitor response to immunotherapy (desensitization).
Important: If a patient has a known IgE-mediated food allergy, Genova DOES NOT recommend exposure to the food that may cause a reaction.
When testing for food antibodies, it is suggested that the patient eat a variety of foods for 2-3 weeks prior to testing (except for foods that are known to cause severe reactions). Doing so will help to ensure the presence of antibodies to problematic foods.
It is also important to remember that IgE antibodies have a circulating half-life of 1-5 days, so any reaction shows current exposure to the antigen, meaning exposure within the several days immediately prior to collecting the test sample. The circulating half-life of IgG is approximately 21-24 days, which means that by approximately 3 months, antibodies to a particular food may be absent if the food has not been consumed by the patient. In other words, if the patient has not consumed the food prior to testing, no reaction to that food would be expected.
When running the Coeliac Profile, it is important to note that antibodies will only be present if the patient has consumed gluten prior to testing. If the patient is already on a gluten-free diet, genetic testing of the HLA DQ2/DQ8 genes may be helpful. According to the American College of Gastroenterology, a proposed gluten challenge after being gluten-free involves eating 3 grams of gluten daily for 8 weeks prior to testing. However, diagnostic changes are seen in most coeliac disease patients after as little as 2 weeks of gluten ingestion.1
It is recommended that a child be at least 1 year old before testing for IgG antibodies in order to eliminate the possibility of maternal antibodies influencing the results. Studies are lacking on the transfer of food-specific antibodies and/or the clinical significance of these maternal antibodies measured in the child's serum.
IgE antibodies do not cross the placenta, so there is no age restriction for IgE testing. According to Medscape, "For immunoglobulin (Ig) E-mediated allergy, there is no minimum age for testing, although it is important to consider age-related changes in patterns of sensitization. Sensitization to foods can occur in babies who are only a few weeks old. On contrast, it is unusual to develop sensitization to respiratory allergens before 2 or 3 years of age. Furthermore, in preschoolers, sensitization to indoor allergens (e.g., cat, dog, dust mites) is more common than sensitization to pollens. Considering these patterns, it is certainly reasonable to test children for food-specific IgE in early infancy if the history suggests food allergy."2
Breastfeeding can result in the transfer of maternal IgG and IgA antibodies to the child. However, studies are lacking on the transfer of food-specific antibodies and/or the clinical significance of these maternal antibodies measured in the child's serum.
The immune system continues to develop into childhood. Therefore, the clinical applicability of test results in pediatric patients may be unclear. What may be interpreted as an abnormal result for an adult, may be normal for an infant's developing immune system. This can be the case with other immune testing, including stool calprotectin and stool eosinophil protein X (EPX), where elevations would be expected in a healthy infant, but abnormal in an adult.
Antibody testing may be inaccurate if the patient has liver disease, severe renal disease, protein-losing enteropathy, HIV infection, or other immunodeficiencies. In patients with selective IgA deficiency, coeliac disease testing should include the IgG antibody against tissue transglutaminase (tTG) and deamidated gliadin (DGP) since the IgA antibody may not be detected or may be very low.
Viruses such as Epstein-Barr virus (EBV), rubella, and cytomegalovirus (CMV) can be associated with lower antibody levels.
Results may be skewed in patients with rheumatological pathologies associated with the production of heterophilic antibodies, such as rheumatoid factor (RF).
Diseases associated with a false positive tissue transglutaminase (tTG) IgA antibody on the coeliac test may include type 1 diabetes, autoimmune liver disease, primary biliary cirrhosis, inflammatory bowel disease, connective tissue diseases, and HIV infection. Genetic testing of the HLA DQ2/DQ8 genes may be helpful in these patients.
Review information on the Test Preparation tab above for details on how medications and supplements may impact this test.
Support guides, charts, and additional aids can be found on the Support Materials tab. Additional educational materials can be found in our Learning Library.
Related Products
Symptoms of conditions can overlap. Certain disease states can influence other body systems. Additional testing can help identify those abnormalities.

The GI Effects® Comprehensive Stool Profile provides valuable insight into digestive function, intestinal inflammation, and the intestinal microbiome.
Gain insight into symptoms triggered by food. The IgG and IgE Antibody Profiles are blood tests that measure antibodies to commonly consumed foods and environmental allergens.